In my role at Cadence, I have the privilege of collaborating with Chief Nursing Officers at independent, community hospitals. For too long, they have been on the frontlines of confronting the simultaneous challenges of solving nurse burnout and nurse shortages.
Before sharing their solutions, allow me to communicate the depth of the problem.
- Pre-pandemic, “One third of nurses reported burnout, and turnover was about 17 percent per year. Since the emergence of COVID-19, burnout has hovered around 50 percent among nurses while turnover rates have risen to between 20 and 30 percent.”
- A 2021 Medscape survey of more than 10,000 nurses revealed less 1 in 5 say they are not burned out at all. More than one third say the pandemic has decreased their satisfaction with being a nurse.
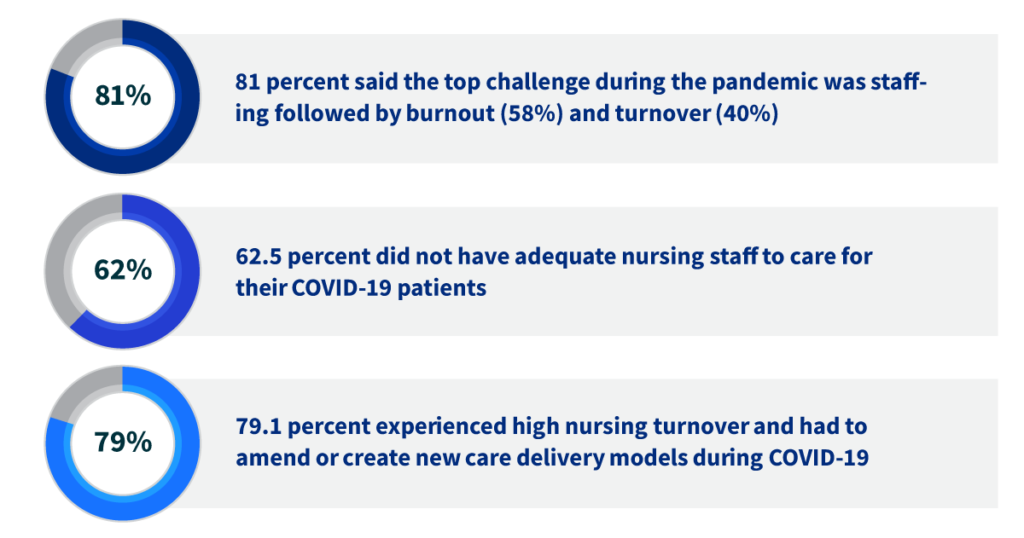
- A late 2021 survey of chief nursing executives found:
As the Chief Clinical Officer for Cadence, my team and I have created a Chief Nursing Officer (CNO) Roundtable to promote peer exchange of what’s working and what isn’t, best practices and efforts around recruitment, retention and recovery – as well as to support each other throughout our respective challenges and successes.
As you might imagine, the COVID-19 pandemic and its impact on frontline nurses is a frequent topic in our meetings. It is during these meetings that we learned of the varied ways these talented CNOs are mitigating nurse burnout and nurse shortages.
Proven Solutions: Nurse Burnout and Nurse Shortages
Heather Hyler, Chief Nursing Officer, Wilson Medical Center, is an excellent example of the care and ingenuity she brings to her role. As we wrote in a recent news release,
“Heather’s success in updating nurse wages has increased the range of healthcare experience offered at WMC, enabling critical patients to stay at the hospital rather than transferring to higher level care facilities. She also has led the hospital’s response to the COVID-19 pandemic, keeping staff updated on CDC guidance, revising protocols, preparing community safety information and helping to make vaccines readily available to the community. As the Kansas Hospital Association reported, “’Heather understood the toll the pandemic was taking on hospital employees, and she brainstormed ways to keep staff positive and engaged through a ‘Who Am I’ employee contest and a weekly ‘Rejuvenation Cart’ filled with treats.’”
Athena Minor, Chief Nursing and Clinical Officer of Ohio County Healthcare, has implemented a number of creative solutions, including:
- Each staff member selects one day per pay period to be on call and receives call pay, saving time when additional nurses are needed. The coordinator evaluates staff for each shift and shuffles assignments and coverage based on skillset.
- The ‘Bring the Best Back Home’ program chooses two juniors and seniors per high school to work in the hospital. These are students who have identified a desire to pursue health careers. They are paid as interns (working 10-15 hours per week) and work around their high school academic and sports schedule to assist with tasks in the areas of their chosen future profession.
- A unique staffing model that has helped decrease turnover and saved the hospital money has nurses in full-time salaried positions give up some benefits in exchange for more paid time off. They commit to a certain number of hours per year but have variable hours per week. They also have the flexibility to switch time with other staff to have more control of their schedule and help with work-life balance. Nurses are paid a salary with a higher hourly wage but work less hours in lieu of benefit time. The offset of cost for increased hourly wages comes from the decreased expense in benefit time and decrease in PRN/Agency pay to fill open positions
As Nursing Leaders and Nurse Executives, we have the opportunity to come together to make improvements for our healthcare workforce and patients. Other solutions from the Cadence CNO Roundtable are:
- Hiring a certified nursing assistant (CNA) to float and do whatever is needed such as transport labs, answer phones and provide one-on-one care.
- Deploying a team approach to allow registered nurses and support staff to help more patients.
- Creating a script for high school graduates, voluteens and patient experience ambassadors to answer phones and call lights and take messages.
- Leveraging task-based nursing such as distributing medications or turning patients versus patient assignments.
- Strengthening connections with nursing schools by hiring and paying students while they are doing their clinical hours and recruiting new nurses before they graduate. Another hospital is repaying nursing school costs and supporting licensed practical nurses (LPNs) who are pursuing registered nurse (RN) degrees.
Despite the challenges nurses and Chief Nursing Officers are facing, I am encouraged by nurses’ commitment to patient care and the mission of healthcare. The 2021 Medscape survey, for example, found more than 90 percent say they are glad they became a nurse, and more than 70 percent said if they could do it over, they would still choose to be a nurse.
I couldn’t agree more.


